February 25, 2000, was an unseasonably warm day that was destined to be a day I would never forget, not because of the warm sunny weather, but because of the storm that was brewing inside my husband’s chest. A week earlier, my husband Larry got up on a Friday morning and could not walk on his right foot. The foot was swollen and red and it was traveling up his leg. I took him to the ER where he was diagnosed with cellulitis and sent home with an antibiotic. Two days later we were back at the ER after he experienced severe chest pain. EKG looked fine, vitals were fine but they admitted for more testing to the telemetry unit. Knowing that cellulitis, (blood poisoning) could travel to the heart, I asked one of the doctors if anyone was checking him for endocarditis, I received a stare like I had just grown a second head and the he walked away.
The next day Larry was given an echocardiogram in his room. The admitting doctor was there, a staff cardiologist. He spoke to us and said, “You have a serious problem, very serious, you have aortic stenosis. You will need a stress test. I need you to come to my office on Friday for the test.” Aortic stenosis? I knew what that meant and I was shocked. Larry had always been fairly healthy and never showed any signs of a heart condition. Where in the world was this coming from?
The doctor sent Larry home the next day with a bottle of nitroglycerine and was told to return to the ER if he experienced any chest pain that would not go away with the nitro. He had five days to wait until he took the stress test and was to remain at home to rest.
The following week the foot began to heal and Larry never complained about any chest pain. Little did I know at the time that he was hiding the pain from me. Gallant as it may have seemed to him to protect me, it could be deadly for him.
During this same week we got word that Larry’s mother was diagnosed with ovarian cancer and not expected to live very long. Her doctor set her up with hospice which was to start that Friday. Larry was her power of attorney and thought it best to discuss her health care with his siblings so we all met at his mother’s on Thursday night. Mom wasn’t sure what was going on; she had been confused for months, and we all thought it was the onset of Alzheimer. Just less than a month earlier, during a routine exam, her gynecologist found a mass in her abdomen. She had an ultra-sound and then a visit to three more doctors before one of them said she had ovarian cancer. He told us to take her home to die. All of those months with her confusion, never complaining of pain, left us shocked to learn she had a mass growing inside of her that would eventually take her life.
I sat on the couch with Mom as we discussed what the doctor had said. For the first time in a long time, she seemed to understand what was happening. We hugged, we cried, we even laughed to try and keep things light. Larry met with some of his siblings and as he knew his health was failing, he requested that his niece, who was second executor of Mom’s will, to be prepared to handle her affairs. He had lost a lot of weight, his face was drawn, his skin was ash, and he walked like an old man, yet he was only 51.
We left Mom on the sofa that night, our hearts breaking, but we had to go and face another mountain that was soon to overwhelm us.
The next morning we sat at the breakfast bar and we both knew that Larry would wind up in the hospital that day. He could barely walk across the room without losing his breath and collapsing. I still did not know that he had been experiencing chest pain the whole week.
As we sat in the doctor’s waiting room, he began to have so much chest pain that he took a nitro in front of me. He finally admitted to taking many others during the week. The pill he took did not help so he took another. I got up and told the receptionist, no one came. A while later, he took a third pill, still no relief. At this point I was becoming annoyed and told the receptionist to go get a doctor. Shortly afterward two nurses came and got him. They told me stay in the waiting room and I would be called if I was needed. I sat nervously, watching and not watching TV, flipping through magazines, walking the floor when finally a doctor approached me and told me that Larry was very ill and that I needed to take him to the ER immediately, a team of doctors were waiting for him. He said that Larry had a severe aortic stenosis. I was a surgical technologist, I knew what he meant and it scared me to death.
Larry appeared with two nurses, one on each side of him, holding him up as they walked him to the door. That is as far as they went. I helped him to the car, a good 200 feet away. The hospital was less than a mile away so I rushed as fast as I could. I pulled up in front the ER drop off and helped him inside. I yelled for a wheelchair and told the triage nurse who he was and she quickly took him to where the doctors were waiting. Now it was my time to wait. A million things seemed to run through my head. I tried to look at it medically, what was the worst scenario, I asked myself? No-I can’t go there. I paced the floor, I walked outside, I tried calling our two sons but could not get in touch with either one. I ran back into the ER looking for a doctor, I could not wait any longer; I had to know how he was. Finally a doctor approached me. The same one that admitted him the week before. He said, “Your husband is very bad, he has an aortic dissection!”
OK, that did it- this was getting worse. He told me that Larry was going to be transferred to another hospital where he would have to undergo emergency surgery. I knew that, I knew that if his condition worsened, Larry would not survive. They let me see him. He was mumbling, incoherent. They had just performed a TEE, transesphogeal echocardiography. This means they used a device that went down his esophagus to the cardiac sphincter and took a picture of what was going on. They found the dissection and knew that this hospital was not equipped to handle this kind of emergency. I ran outside to try and contact my sons once more and got in touch with my youngest, Craig. I told him what happened and he said he would meet us at the hospital. I talked to my mother almost hysterically. Amazing how as parents we try to stay calm in front of our children but when we are the child, it seems okay to break down. My mother tried to console me as best she could. Before I hung up from her, the EMTs were wheeling Larry out and into the ambulance. He was escorted by the RN that was on the case and one of the interns. I climbed into the front seat of the cab as a police car escorted us down the highway. Several miles away another police car waited at a busy intersection where he had stopped traffic so we could go through without delay. The ride seemed to take forever, especially when we hit the traffic in the city. We had to drive over median strips to get around it. We finally arrived and they rushed Larry to the Cath Lab.
I was told they were going to perform a catherization. I thought that was wasting time. What were they thinking, the dissection could separate completely at any time and he could bleed to death! They sent me to a waiting room two floors away and said they would call me. As I sat there, trying to take it all in I noticed the medical crew leaving that had brought Larry in. I heard the nurse say to the intern, “His EKG and vitals were fine the whole time, can you believe that?”
I sat in the waiting room for about 10 minutes when I walked out into the hallway and saw my youngest son coming. He grabbed me and hugged me so hard I thought I would break. With tears in his eyes he asked how his Dad was. I told him what I knew and just then someone called my name. The waiting room had a phone and someone had called me to report on Larry. I answered the phone and they told me to return to the lab where I could see Larry. We raced to the lab and were waiting when they brought him out. He was in so much pain. They had given him morphine but it didn’t help. He kept saying, “It hurts, can’t you give me something, it hurts.” There was blood on the sheet where they had placed the lead through the groin and I could see my son starring at it and becoming more and more pale. Craig, was never one to react to the site of blood well, it always upset him.
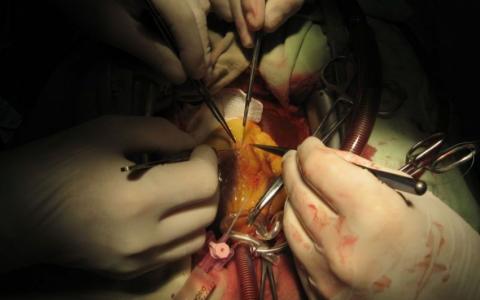
The cardiologist that performed the catherization approached us as said that Larry had two blocked arteries and he would be taken to the operating room immediately. He said that Dr. Kuchler was on duty and we were lucky because he was the best heart surgeon they had. Dr. Kuchler then came over and introduced himself and I asked, “Are you as good as they say you are?” He smiled modestly. “Then go save my husband.”
The rest of evening was full of phone calls to family, praying in the sanctuary, pacing the floor, crying, and more praying. The night had brought the cold February breeze in. I didn’t have a coat on because when we left for the doctor’s office it was so warm. Hours passed and I got a phone call from the OR staff, they had grafted the two arteries and were testing the valve now; it would be several more hours. More waiting. By then my sister and her husband had arrived and one of Larry’s three brothers. He only stayed a couple of hours because my mother-in-law was not doing well either.
Finally around 11:00 pm, seven hours after we arrived at this hospital, Larry was out of surgery-alive! He was taken to CCU where we met with the surgeon. Sometimes it is harder to hear the medical jargon about a loved one, when you know what they are saying when you are aware of the terminology and how things work. You not only understand, you know what can go wrong, you know how it might end. My sister, standing by my side, a registered nurse who worked CCU, knew all too well what the doctor was saying. He told us that Larry had endocarditis and that the vegetation had invaded the chambers of his heart, his aortic valve, as well as the tricuspid and mitral valves. They replaced his aortic valve with a tissue valve because there just wasn’t enough healthy tissue left to stretch. They had to use part of his pericardium tissue (the protective covering over the heart) to patch his heart. They wanted me to be prepared that he may have to return to the OR.
If you have ever been dazed by a sudden jolt, you will understand the response to this news. Having a million questions in my head, I did not ask one. I stood there, dumbfounded. How could this be?
I stood by my husband’s bed, watching him on the ventilator, holding his hand and praying for his recovery. My son stood by, tears running down his face, tightening his lips like his Dad does when he is upset. The night was long, but he survived. They did not have to take him back to the OR. By 1:00 am, he was off the ventilator. The next morning they sat him up in the bed. The medical staff was amazed at his progress so soon. Two days later he was transferred to the step-down unit and the following day his mother died.
I can not say that my husband’s recovery was without set-backs. The infectious disease physician worked diligently to come up with a treatment to attack the bacterial infection in his heart. The surgeons did their best to remove all of the abscesses but he was still left with some. They inserted a tube into an artery that went to his heart called a Hickman catheter, that would deliver the vital antibiotics and fluids he needed for the next couple of months.
His will to get better and to see his mother one more time, got him an early release by the doctors with the promise that he would rest and follow his treatment plan. They let him go home the day of his mother’s viewing. I took him that evening for a private viewing, but he was instructed not to attend the funeral.
Larry convalesced for four months. During that time he experienced kidney failure from the strong antibiotic regimen but he beat that too. He returned to work only to discover months later that his strength was never going to be the same and he could no longer do his job so he moved on to something else, still a fighter, still a winner.
Follow-up:
There are two things that could have caused the infection in his heart. One, he worked at an oil terminal and stood in contaminated water. His boots were soaked and he had a cut on his foot. Later his foot became infected and the infection could have traveled to his heart. He also had his teeth cleaned several weeks before. If someone has a prolapsed heart valve, they should always take antibiotics before having their teeth cleaned. Larry was never diagnosed with a valve problem so it is more likely that the cellulites in his foot traveled to his heart. Endocarditis carries a very high mortality rate but Larry beat the odds. Even with the extreme damage that was done to his heart, eight years later, his pig’s valve is still working. He is monitored often and will eventually require surgery to replace the aortic valve but that’s another story.